Laparoscopic Adrenalectomy
Minimally Invasive Surgical Removal of the Adrenal Glands
The adrenal glands are part of the endocrine system and are located just
above the kidneys. Adrenalectomy, or removal of the adrenal gland, may be
necessary when patients have adrenal masses, either benign or malignant.
Many of the benign adrenal tumors secrete hormones that can result in high
blood pressure, headaches, heart palpations, as well as other symptoms and
need to be removed. However, in many cases patients can feel completely
normal. Most benign and malignant masses or tumors can be removed
laparoscopically.
Traditional open surgery involves making an 8-20 inch incision in the flank
or abdomen and in some cases removing a rib. Postoperative pain and
numbness near the wound site can interfere with breathing and extend
recovery. Laparoscopic adrenalectomy, using tiny "keyhole" incisions,
offers similar cure rates but with decreased blood loss, a shorter hospital
stay and recovery period, as well as decreased pain and infection rates.
The procedure
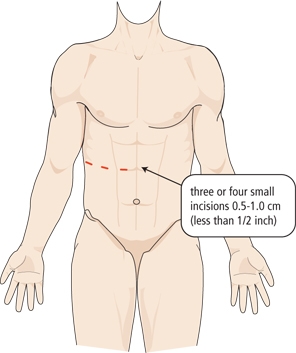
Under general anesthesia, trocars (cylindrical tubes) are placed into the
abdominal cavity through 3-4 tiny incisions, ~1/2 inch, to allow "insertion
of the laparoscope. Next, carbon dioxide injected through one of the
incisions enlarges the cavity and separates the abdominal wall from other
organs. A laparoscopic camera provides a magnified view, making it possible
to identify vessels and structures very clearly.
Thin surgical instruments then are inserted. The kidney and either the
spleen or liver are mobilized to provide better access to the adrenal
gland. Once the adrenal gland is freed from surrounding structures, it is
extracted and removed through one of the incisions. The wounds are then
closed and sutured. The tissue is sent to a pathologist for examination.
Potential Risks and Complications:
Although this procedure has proven to be very safe, as in any surgical
procedure there are risks and potential complications. The safety and
complication rates are similar when compared to the open surgery. Potential
risks include:
Bleeding: Blood loss during this procedure is typically minor (less than
100 cc) and a blood transfusion is needed in less than 5% of patients.
Infection: All patients are treated with intravenous antibiotics, prior to
starting surgery to decrease the chance of infection from occurring after
surgery. If you develop any signs or symptoms of infection after the
surgery (fever, drainage from your incisions, urinary frequency/discomfort,
pain or anything that you may be concerned about) please contact us at
once.
Tissue / Organ Injury: Although uncommon, possible injury to surrounding
tissue and organs including bowel, vascular structures, spleen, liver,
pancreas, kidney and gallbladder could require further surgery. Injury
could occur to nerves or muscles related to positioning.
Hernia: Hernias at incision sites can occur, but are very rare, since all
keyhole incisions are closed carefully at the completion of your surgery.
Conversion to Open Surgery: The surgical procedure may require conversion
to the standard open operation if difficulty is encountered during the
laparoscopic procedure. This could result in a larger standard open
incision and possibly a longer recuperation period.
During your hospitalization:
Immediately after the surgery you will be taken to the recovery room, then
transferred to your hospital room once you are fully awake and your vital
signs are stable.
Postoperative Pain: Pain medication can be controlled and delivered by the
patient via an intravenous catheter or by injection (pain shot)
administered by the nursing staff. You may experience some minor transient
shoulder pain (1-2 days) related to the carbon dioxide gas used to inflate
your abdomen during the laparoscopic surgery.
Nausea: You may experience some nausea related to the anesthesia.
Medication is available to treat persistent nausea.
Urinary Catheter: You can expect to have a urinary catheter draining your
bladder (which is placed in the operating room while the patient is asleep)
for approximately one day after the surgery. It is not uncommon to have
blood-tinged urine for a few days after your surgery.
Diet: You can expect to have an intravenous catheter (IV) in for 1-2 days.
(An IV is a small tube placed into your vein so that you can receive
necessary fluids and stay well hydrated; in addition it provides a way to
receive medication.) Most patients are able to tolerate ice chips and small
sips of liquids the day of the surgery and regular food the next day. Once
on a regular diet, pain medication will be taken by mouth instead of by IV
or shot.
Fatigue: Fatigue is common and should start to subside in a couple weeks
following surgery.
Incentive Spirometry: You will be expected to do some very simple breathing
exercises to help prevent respiratory infections through using an incentive
spirometry device (these exercises will be explained to you by the nursing
staff during your hospital stay). Coughing and deep breathing is an
important part of your recuperation and helps prevent pneumonia and other
pulmonary complications.
Ambulation: On the day of surgery it is very important to get out of bed
and begin walking with the supervision of your nurse or family member to
help prevent blood clots from forming in your legs. You can also expect to
have SCD's (sequential compression devices) along with tight white
stockings to prevent blood clots from forming in your legs.
Hospital Stay: The length of hospital stay for most patients is
approximately 1-2 days.
Constipation/Gas Cramps: You may experience sluggish bowels for several
days following surgery as a result of the anesthesia. Suppositories and
stool softeners are usually given to help with this problem. Taking a
teaspoon of mineral oil daily at home will also help to prevent
constipation. Narcotic pain medication can also cause constipation and
therefore patients are encouraged to discontinue any narcotic pain
medication as soon after surgery as tolerated.
