Diabetes and Your Feet
BIDMC Contributor
JULY 31, 2019
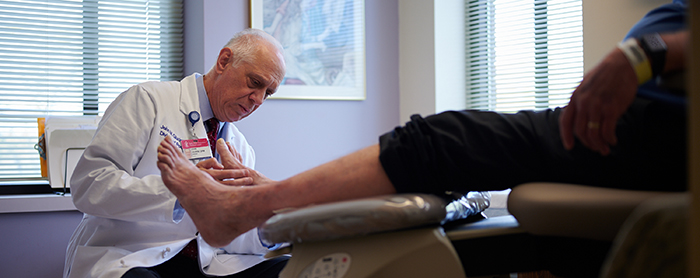
Diabetes can cause problems with your feet. Read below to hear from John Giurini, DPM, Chief of Podiatric Surgery, to learn about these complications and how experts at Beth Israel Deaconess Medical Center (BIDMC) can help you.
How can diabetes impact the feet?
Diabetes is a serious disease that affects various parts of your body. In terms of the feet, it can lead to nerve damage, causing a loss of sensation in your foot. It can also affect blood supply to your feet, making it difficult for injuries to heal.
What is diabetic neuropathy?
Diabetic neuropathy is one of the most common complications of diabetes and can present in a few different forms. The first way is a lack of sensation in the foot, making it difficult to feel any sores, blisters or injuries, even if you’ve stepped on something sharp.
Another form of neuropathy occurs when the nerves that control muscle function are affected. These patients will have trouble walking and may develop what is referred to as a “drop foot” that makes tripping or falling more common.
The third form of neuropathy is called neuritis or painful neuropathy. These patients have constant foot pain throughout the day, and in more severe forms, can keep them awake at night. We often refer patients to BIDMC’s Arnold-Warfield Pain Center to help treat this type of neuropathy.
What is peripheral vascular disease?
Peripheral vascular disease is the narrowing of arteries, which affects the blood flow to limbs. Blood flow is important to bring nutrients such as oxygen and growth factors to the foot to allow sores to heal. With poor circulation, sores and cuts heal more slowly. We look for this condition in patients with diabetes because diabetes-related nerve damage can make it difficult to diagnose. We often refer these patients to our Division of Vascular and Endovascular Surgery for evaluation and treatment.
What can I do to protect my feet?
The earlier you catch a problem, the easier it is to treat. It’s important for patients with diabetes to get into the habit of regularly inspecting their feet. The best time is immediately after a shower while drying your feet or at the end of the day when removing socks and shoes. If you see a blister, it’s important to get off the foot completely, put a clean dressing with some type of antiseptic on it, and contact your podiatrist or physician.
Another good habit is to inspect your shoes before putting them on. Many times things get inside shoes - rocks, pebbles, etc. that can cause irritation of the foot. With lack of sensation, you may not be able to feel these objects.
Finally, high-risk patients should be seen by a foot care specialist every three months. High-risk patients include those with abnormal sensation or circulation, or those with foot deformities. Many of these problems can be prevented by controlling your diabetes and inspecting the feet regularly.
Learn more about diabetes and podiatry services at BIDMC.
